Today we’ll answer the 7 most important questions related to heat injuries at the job site.
We’ll give you some points on what it is, how to identify it and some ways your organization can increase awareness and preparedness.
So whether you’re a newly minted Certified Safety Professional (CSP) or a grizzled industrial hygiene veteran, we hope you get a lot of good info.
- What is heat stress?
- What causes a heat-related injury?
- How to determine the heat level of a work site?
- Does workload affect my team’s core temperature?
- How hot are my workers getting?
- What are the symptoms and types of heat stress?
- What makes up a great heat-related illness prevention program?
What is heat stress?
Simply put:
Heat stress occurs when accumulation of heat inside the body outpaces its ability to dissipate.
This heat stress can occur from accumulated heat either made internally by the human body’s physiological processes, especially the work done by muscles, or absorbed externally in an environment like those working in the summer sun or in a hot smelting plant. As heat accumulates, the body must work to dissipate and help maintain thermoregulation. As more heat stress is introduced to the body, it can eventually become unable to dissipate at a sufficient rate to maintain a safe internal temperature.
Any number of medical conditions collectively known as heat related injuries can occur if the level of heat stress on an individual is sufficient. Heat related injuries span a spectrum from nominal to severe.
Spectrum showing spectrum of heat injuries from rash to stroke
source: SlateSafety.co
At the lower end of severity are heat rashes and heat cramps. These are some of the earliest manifestations of too much heat stress on the body. Without proper intervention, heat exhaustion can proceed to heat stroke which can damage the brain as well as other vital organs and even cause death.
What causes a heat-related injury?
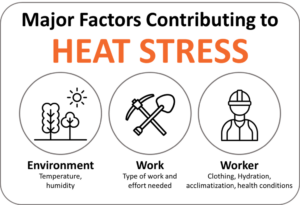
Broadly speaking the major contributing factors to heat stress can be grouped into the environment, the worker and the work. Understanding these three factors can help:
- The environment
- The work
- The worker
Source: SlateSafety.com
A heat-related injury occurs when the body’s normal mechanisms are unable to effectively regulate its internal temperature. Typically, at high temperatures the body’s primary effort to cool itself occurs through the evaporation of sweat. Under certain conditions; however, this cooling system becomes less effective. When air surrounding the body has a high level of humidity sweat cannot evaporate as quickly, preventing the body from releasing heat effectively. Additionally, without proper fluid intake, excessive fluid loss and electrolyte imbalance may lead to dehydration. In these cases, a person’s body temperature rises rapidly.
There can be additional factors that limit the ability of the body to regulate temperature. Things such as age, obesity, fever, dehydration, heart disease, poor circulation and drug or alcohol use.
How to determine the heat level of a work site?
Understanding the environment of a work area really lays the backdrop for understanding how to prevent and mitigate heat stress. The heat measurements of the site should be taken either directly at the work site or as close to the work site as possible. For jobs that require a worker to move between different zones or locations, the heat measurements should be taken at each individual area and during each period of constant heat levels where workers are exposed. Worker task zone heat profiles should be generated to understand variations and set threshold limits.
Generally speaking, the best approach in determining environmental heat is to use the Wet Bulb Globe Thermometer (WBGT) method. The U.S. Army was one of the earliest users of WBGT and the method is widely accepted to provide the most accurate estimation of heat by taking into account 5 different variables in its equation.
The WBGT takes into account 5 factors:
- Temperature
- Humidity
- Wind speed
- Sun angle
- Cloud cover (solar radiation)
Additional, methods such as Corrected Effective Temperature (CET), or Wet Globe Temperature (WGT) can be used and then converted to an approximation of WBGT. A more detailed dive on WBGT can be found at Korey Stringer Institute.
With WBGT, training officers, safety managers and industrial hygienists can manage their workloads effectively and help optimize performance in high-temperature environments.
Does workload affect my team’s core temperature?
Absolutely!
With a better understanding of how to collect the heat level of an environment, let’s take a look at how the type of work can increase the risk of heat injuries and the effort needed to reduce the impact.
As a workload becomes more challenging, more muscles are recruited to perform. The higher the workload (intensity and duration), the more body heat is generated. The heat generated by these muscle groups is transferred via the conductive heat exchange between the working muscles and blood to the core, resulting in an increased body temperature. In short, the more rigorous the work and the longer it lasts the more your core temperature will increase.
Understanding what type of work is being achieved helps determine a safe zone to complete it in. There are a few different methods for evaluating the work type of an individual in hot environments.
Here are a couple of the most common formulas for determining work load based on environmental heat:
- NIOSH has a handy guide to help and urges that employers should seek to ensure that their workers are not exposed to combinations of metabolic and environmental heat greater than the applicable Recommended Alert Limits (RALs) and Recommended Exposure Limits (RELs)
- OSHA has a similar method used to determine the metabolic work rate.
How hot are my workers getting?
That’s a great question for worker safety. Now that we have an understanding of how to measure the work environment and we know that different types of work can contribute more to heat stress, let’s take a look at understanding how to measure the heat generated by the worker to help with heat-related illness prevention.
As a worker performs activities, their muscles generate heat, this heat produced is called metabolic heat (put a fancier way, metabolic heat is a by-product of muscular metabolism). Finding the metabolic heat of an individual can only occur in two ways — direct and indirect calorimetry — and they both need to be performed in a laboratory setting. Fortunately, the National Institute for Occupational Safety and Health (NIOSH) recommends an alternative to gauge how your team is doing: physiological monitoring (e.g. equipping sensors for Heart rate, core body temperature, and body water loss, etc…).
With recent advances in remote physiological monitoring, the right balance between accuracy and practicality are being found.
Now that you understand what heat stress is and where it comes from. Let’s look at the different types of heat stress.
What are the symptoms and types of heat stress?
Because types of heat-related illnesses can vary in severity it’s important to understand the possible progress of an injury and intervene at the earliest level. An increase in a body temperature of two degrees Fahrenheit can affect mental functions. A five degree Fahrenheit increase can result in serious illness or death. For workers in hot environments or during hot weather, a heat injury may be an underlying cause for other types of injuries like heart attacks, falls and equipment accidents.
Heat Rash
Heat rash is a more mild form of a heat related injury and occurs in hot humid environments. It occurs when sweat ducts become blocked from profuse sweating. It can occur at any age but is most prevalent in children.
- Signs of heat rash: Heat rash often appears as a cluster of small red pimples or blisters. The skin irritation can be itchy and it typically occurs on the neck and upper chest, in the groin, under the breasts, and in the elbow creases.
Heat Cramps
Often associated with heavy perspiration most notably during strenuous activities heat cramps are the body’s response when sweat depletes needed internal salt and moisture levels. As the body loses these electrolytes it can lead to painful muscle cramps, often following exercise. Heat cramps may also be a symptom of heat exhaustion.
- Sign of heat cramps: Heat cramps most often present in the abdomen, arms, or legs following strenuous activity. If the affected person has heart problems or are on a low sodium diet, seek medical attention for heat cramps.
Heat Syncope (fainting)
Heat syncope is a fainting episode that can occur in the heat when your body, in an effort to cool itself, causes the blood vessels to dilate to such an extent that blood flow to the brain is reduced. When a person rapidly rises from prone or sitting positions a fainting spell can occur. It typically occurs in individuals who are not acclimatized to the heat. Dehydration and lack of acclimatization can be contributory factors to heat syncope.
- Signs of heat syncope: dizziness or lightheadedness and fainting, generally due to prolonged exposure to heat, dehydration, or orthostatic hypotension.
Heat Exhaustion
Heat exhaustion is the body’s response to an excessive loss of water and salt contained in sweat as a result of engaging in physical activity (work or exercising) in a hot environment. The body temperature may be normal or mildly elevated, but not above 104 F (40 C). It often occurs in individuals who are not accustomed to working or exercising in the heat.
- Signs of heat exhaustion: nausea and vomiting, headache, muscle cramps, weakness, and profuse sweating.
Heat Stroke
The most severe form of heat related injury, heat stroke, can lead to death or permanent disability. Heat stroke occurs when the body’s temperature rises rapidly in excess of 104 F (40 C). With such a quick rise temperatures at this level can quickly damage the brain and other vital organs. Generally, the extent of injury depends on the duration of exposure to excessive heat and the peak temperature attained. Heat stroke is sometimes referred to as sunstroke.
- Signs of heat stroke: high body temperature (above 104 F or 40 C), skin that is red or hot, either moist or dry skin (sweating may have stopped), rapid heart rate, difficulty breathing, headache, dizziness, loss of coordination, nausea and vomiting, confusion and restlessness, seizures, and unconsciousness/coma.
What makes up a great heat-related illness prevention program?
A vigorous heat-related illness prevention program is a multi-pronged approach that minimizes the impact on a workforce’s exposure to heat related illnesses and injury.
The OSHA Technical Manual Section III: Chapter 4 helps highlight what a successful heat-related illness prevention program could look like. It has four main pillars:
Acclimatization Program
A great program begins with preparation. For a workforce that performs in hot work zones, implementing a heat acclimatization program is a must.
Heat acclimatization occurs over a period somewhere between 7-14 days with a methodical, incremental approach where environment and exposures are sufficiently stressful to invoke profuse sweating and elevated body temperatures but not to a point of heat exhaustion. Generally speaking a slower, more methodical approach will achieve the best results in a workforce.
Medical Monitoring Program
Strong heat-related illness prevention programs are able to factor in a worker’s individual medical needs as well as interpret the aggregate needs of an organizational workforce at scale. A properly set up medical monitoring program seeks to evaluate workers before, during and after risk exposures and look for ways to mitigate any unnecessary impact on the physiology of an individual.
Properly equipped programs that provide accurate measurement for monitoring the health of a workforce (core temperature, hydration, pulse, blood pressure, etc.) drive conversation around what is or is not working in a program and how to effectively support the workforce.
Training Program
Just like many safety topics, awareness and action are key to maximizing effects. Providing your organization’s workforce with a clear understanding of preparedness for hot work ensures adequate knowledge and demonstrates leadership’s buy-in to safety.
Typical training sessions should include topics such as how to spot symptoms in co-workers, understanding proper hydration, and understanding what other factors that can contribute to heat stress. Additionally, adequate training reserved for manager staff on proper weather reports, how to use adjusted temperatures (heat index, humidex or WBGT) to effectively make decisions.
Take a look at the OSHA Heat Illness Prevention Training Guide that outlines an approach to material. It also provides flexibility to deliver the training in either one 45-minute training session or three 15-minute sections to cover: Health effects of heat, How to respond to symptoms and Preventing heat illness.
Heat Warning System
A heat warning system (HWS), heat health warning system (HHWS) or heat alert program (HAP) is an action plan set in place to help notify a group of individuals, whether at the community, organization or worksite level of an impending heat wave and to begin to help to minimize the risks associated with it. There is increasing evidence that heat warning systems are effective in reducing mortality and even morbidity rates during a heat wave.
Included in an effective heat warning system are thoughtfully implemented plans ranging from short-term warnings, advisories, cooling shelters and “buddy” checks to longer-term plans such as improving building and living environments. In general, an effective heat warning system has these components:
- Weather forecasts such at those from the National Weather Service
- A system for determining how weather patterns may impact a range of health outcomes
- A spectrum of thresholds and actions
- A mechanism for alerting the areas impacted, whether those areas are widespread or targeted